Whether you were recently diagnosed with Type 1 diabetes or need to begin taking insulin for Type 2 diabetes, the idea of managing diabetes with insulin injections can be scary. Here’s what you need to know about using insulin, including information about the different discounted insulins available through Simplefill’s prescription assistance program.
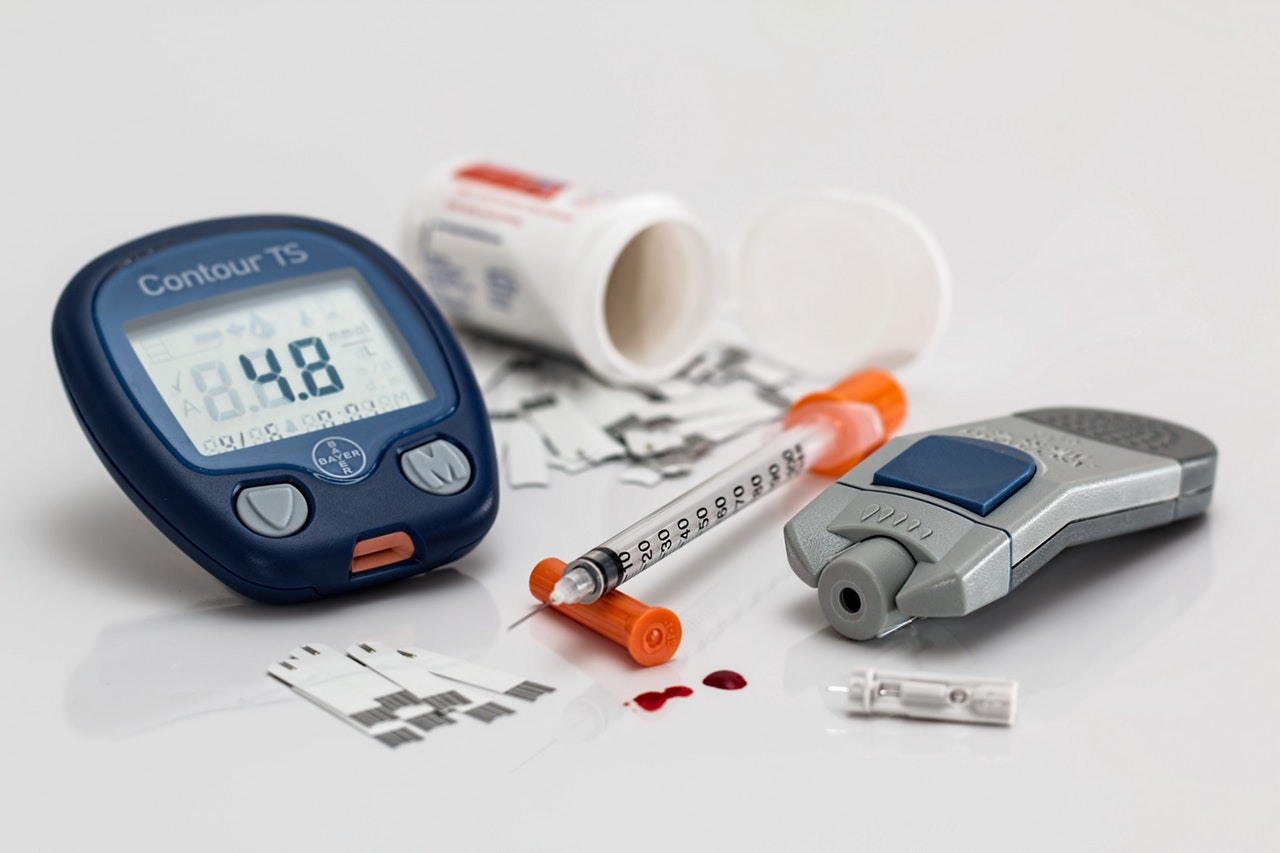
Insulin Delivery Methods
While most diabetics use a needle and syringe, other methods of insulin delivery are becoming increasingly popular. Insulin pens, for example, contain a cartridge, a dial to measure dosage, and a disposable needle. Insulin pens are more accurate to use, and many people find them simpler and more convenient as well. Insulin pumps, while more expensive, are connected to your body through a catheter. They deliver slow-acting insulin to regulate blood sugar between meals and bolus doses after eating. Many companies already provide oral diabetes medications for people not dependent on insulin, and oral insulin is just around the corner.
The Importance of a Healthy Diet
No diabetes management strategy is complete without a plan for healthy eating. In addition to eating healthy carbohydrates, good fats, fiber-rich, heart-healthy foods, it’s also important for people with diabetes to eat three meals a day at the same time of day. Talk to your doctor about how an improved diet can help manage your diabetes.
How to Take Insulin
While you should go over insulin instructions more thoroughly with your doctor, this helpful guide covers some insulin basics for people using needles and syringes and can serve as a great resource for anyone new to managing diabetes with insulin.
Store Your Insulin Properly
Storage is the first step to an effective insulin injection. Because every brand is different, you’ll want to check the storage instructions on your prescription, but there are some good general rules to follow. Insulin you’re currently using can be stored at room temperature. Avoid storing insulin in the bathroom or in direct sunlight, as this can cause the insulin to overheat, making it less effective. Insulin you aren’t currently using should be stored in the refrigerator.
Check Expiration Dates
Each bottle of insulin will have its own general expiration date and length of longevity after opening. We recommend writing the date on a bottle when you open it, so you can be sure you know when to stop using.
Use Alcohol Wipes
Before your insulin injection, be sure to clean the area you plan to inject with alcohol and wait until it dries before injecting. If you’re using a vial or syringe, doctors also recommend cleaning both rubber stoppers with alcohol.
Choose Your Injection Site Carefully
While you’ll want to discuss injection sites with your diabetes care team, it’s generally best to inject in fatty areas of your abdomen, outer thighs, and arms. You’ll also want to regularly rotate injection sites to prevent hard lumps or fatty deposits from developing. This can be done by injecting two inches away from the most recent injection site in that area and by changing injection regions every week.
Don’t Remove Needle Too Quickly
In order to make sure you get the full dosage of insulin, make sure you hold the needle in your skin for 5-7 seconds.
Don’t Reuse Needles or Syringes
Never reuse needles or syringes, as doing so can lead to infections at the injection site.
How to Pay for Insulin
Because prices continue to soar and so many people can’t afford insulin, Simplefill is doing everything we can to help people pay for their diabetes medications. In fact, the team at Simplefill assists thousands of diabetics in affording their insulin each month. Simplefill has prescription assistance programs available for several diabetic medications, including insulins like Humalog, Novolog, Lantus, Levemir, Apidra, Toujeo, and Tresiba. If you can’t afford your medication, give us a call or fill out our online application to find out if you qualify for prescription assistance. In the meantime, check out our blog, where we cover everything from how to pay for prescriptions without insurance to the 2019 changes to Medicare Part D.